| dc.description.abstract | INTRODUCTION: Widespread pulmonary calcification is a relatively uncommon finding in patients presenting with dyspnea; differential diagnosis is limited, particularly when accompanied by a diffuse “sandstorm” appearance on plain radiographs. Pulmonary alveolar microlithiasis (PAM) is an extremely rare genetic disease characterized by deposition of calcium phosphate microliths choking the alveoli and small airways.
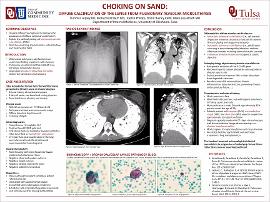
CASE DESCRIPTION: A 33-year-old female immigrant from the Mediterranean region presented for acute on chronic dyspnea. Her 10-year history of exertional dyspnea was punctuated by two days of acute, unremitting, exertional and resting dyspnea with associated fever, pleurisy, and anxiety. Initial room air oximetry was 68%, increasing to 92% on 2L supplemental oxygen. Exam showed cachexia, tachypnea without accessory muscle usage, and diffuse bronchial breath sounds. Laboratory evaluation revealed polycythemia, and computed tomography showed essentially complete lung opacification with diffuse confluent sand-type calcific opacities with air bronchograms. Extensive inpatient workup for a precipitating infectious or rheumatologic etiology of acute decline was largely fruitless, including blood and sputum cultures, atypical respiratory panel, fungal cultures, and autoimmune workup. Quantiferon gold testing was positive. Bronchoalveolar lavage showed scattered calcified concretions. She was discharged on supplemental oxygen to follow up with an interstitial lung disease specialist and complete latent tuberculosis treatment. She was unfortunately lost to follow up after returning to her home country.
DISCUSSION: Lung tissue calcification can be organized into three main categories: metastatic calcification (i.e., deposition in normal tissue due to systemic disease); dystrophic calcification (i.e., deposition due to trauma or previously abnormal tissue), and PAM – a rare genetic mutation producing an abnormal type IIb sodium phosphate cotransporter in alveolar type II cells, from mutation of the SLC34A2 gene1. The dysfunctional cotransporter fails to clear phosphate from degraded surfactant, resulting in microlith accumulation, chronic inflammation, tissue destruction, pulmonary fibrosis, and respiratory failure2,3. PAM has been diagnosed in 65 countries and is most common in Asia. There is a spectrum of disease severity; some patients present asymptomatically, discovered based on incidental abnormal radiographs, and some present in respiratory failure. CT chest plus bronchoscopy with bonchoalveolar lavage is typically used for diagnosis. Clinical course varies but most patients progress to respiratory failure and cor pulmonale. Currently the only definitive treatment is lung transplantation1.
Widespread or multifocal calcification is rare. When diffuse alveolar calcific disease is present, the differential should include metastatic pulmonary calcification and pulmonary alveolar microlithiasis. In our patient, progression of her underlying lung pathology was suspected as etiology of progressively worsening dyspnea. | en_US |