| dc.description.abstract | BACKGROUND: Transitioning patient care to primary care physicians after pediatric hospitalization plays a critical role in children’s health. Follow-up appointments are an ideal time to provide education, address concerns, and arrange for continuity of care.
This quality improvement (QI) study aimed to improve the percentages of primary care clinic follow-up within 7 days of hospital discharge.
METHODS: Using the Plan-Do-Study-Act (PDSA) Model for Improvement, a multidisciplinary team examined pre-implementation data for patients discharged from the children’s hospital in February 2018. Electronic medical record (EMR) review was performed to determine if follow-up appointments were scheduled and attended within 7 days of discharge. Four week PDSA cycles were then completed by the medical residents, pediatric hospitalists and a care transition coordinator. Cycle 1 (n=25) involved developing an EMR-based shared patient list to identify all patients needing follow-up. In Cycle 2 (n=69), monthly standardized resident education was implemented to optimize use of the shared patient list. In Cycle 3 (n=81), a discharge appointment template was used to schedule appointments for patients discharged on weekends.
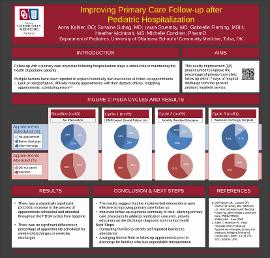
RESULTS: Percent of appointments scheduled increased throughout the PDSA cycles from baseline (baseline - 60%; cycle 1 - 72%; cycle 2 - 74%; cycle 3 - 85%), as well as percent of appointments attended (baseline - 56%; cycle 1 - 56%; cycle 2 - 61%; cycle 3 - 70%) with p<0.001. Clinic follow-up was lower for patients with chronic illnesses but did improve from cycle 1 (42%) to cycle 3 (67%). The percentage of appointments scheduled for weekend discharges was not significantly different from weekday discharges, and increased from baseline over the course of the PDSA cycles.
CONCLUSION: The number of follow-up appointments both scheduled and attended increased throughout the study, suggesting that the QI measures implemented were effective. Further interventions will focus on patient and system barriers to appointment attendance. | en_US |